Are you dealing with pelvic floor dysfunction? If you’re experiencing urinary issues, discomfort during sex, lower back pain, or pressure in the pelvic region, you might be having trouble with your pelvic floor — but rest assured, you’re not the only one.
It’s estimated that a quarter of women suffer from some kind of pelvic floor dysfunction, and it is often experienced by expectant moms and new mamas — although men can experience the condition, too.
While pelvic floor dysfunction — also called pelvic floor dyssynergia— is a club with more members than you may realise, it’s actually relatively easy to avoid,or at least improve. By better understanding your symptoms and making a few lifestyle changes, dealing with pelvic floor dysfunction is a whole lot easier. Here’s to a better you!
What is pelvic floor dysfunction?
The pelvic floor muscles — including the levator ani and the coccygeus — are muscles in the bottom of your body (which can weaken during pregnancy or become strained during childbirth) that support what we call the “pelvic organs”. Pelvic floor dysfunction is aptly described as “the inability to correctly relax and coordinate your pelvic floor muscles to urinate or have a bowel movement”.
What are the causes of pelvic floor dysfunction?
Pelvic floor problems usually occur as a result of pregnancy and childbirth — mainly due to the strain that’s put on the pelvic floor muscles during pregnancy — but it doesn’t only affect new or expectant moms. All women (and men, too) can experience pelvic floor dysfunction at some point in their lives.
Other causes of pelvic floor disorders might include:
Chronic straining when passing stools
Trauma to your pelvic area (sustained in an accident, for example)
Heavy lifting
Pelvic surgery
Aging (the pelvic floor muscles naturally weaken as we get older)
Being overweight
Whatever the cause of your pelvic floor issues, not being in full control of your pelvic floor can lead to a number of uncomfortable and inconvenient symptoms.
What are the symptoms of pelvic floor dysfunction?
To know for sure that you have pelvic floor dysfunction, you’ll need to get a diagnosis from a doctor or health professional. Bear in mind that it’s much more likely if you’re older, have had multiple births or a traumatic birth, or have chronic health issues that increase pressure in the pelvis.
To diagnose pelvic floor dysfunction, a doctor or healthcare provider will ask you a series of questions — whether you have a history or urinary tract infections, if you experience pain while having sex, and so on — while they’ll also perform a physical exam to see how well you can control your pelvic floor muscles.
According to Medical News Today, “research from National Institute of Health indicates that urinary incontinence, pelvic organ prolapse, or both occur in about half of all women who have given birth and are closely associated with birth-related injury to the pelvic floor muscles”.
Pelvic floor dysfunction usually makes itself known with a few telltale symptoms, such as:
Pelvic pain or pressure
Urinary incontinence (including not being able to fully empty your bladder or hold urine)
A frequent or urgent need to go to the bathroom
Pain when peeing
Constipation, or frequently having to strain to pass a stool
Lower back pain
Pain during sexual intercourse
Between incontinence and discomfort, these symptoms can make everyday life a bit of a drag. However, the good news is that if you’re wondering how to treat pelvic floor dysfunction, there are plenty of effective ways to reduce your pain and give you back control of your life.
How to treat pelvic floor disorders
When it comes to treating pelvic floor dysfunction, there are a number of possible treatment options. However, the most effective way of improving pelvic floor dysfunction symptoms is by strengthening the pelvic floor muscles. This is typically achieved through a series of pelvic floor exercises known as Kegels, which are really simple to learn and can easily be worked into your daily routine.
Pelvic floor therapy at home
The best way to deal with pelvic floor dysfunction and (fingers crossed) even avoid it in the first place, is to establish a routine of Kegel exercises. You can practice these pelvic floor exercises at home, whether you’re a new mum or someone who’s been suffering from pelvic discomfort for a short while.
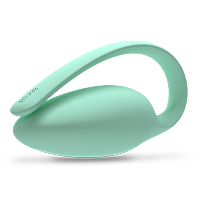
You perform Kegel exercises by lifting, holding and then relaxing your pelvic floor muscles. Using a device like Elvie Trainer can help you stay on track with your exercises and ensure you’re doing them correctly. Elvie Trainer helps you visualise a hidden set of muscles that support everything from core stability to bladder control.
We’re not here to toot our own horns, but at Elvie, we’re considered experts on pelvic floor training.
Over time, Kegel exercises strengthen the pelvic floor muscles, which support the uterus, bladder, small intestine and rectum. Will Kegels completely fix your pelvic floor dysfunction? Well, that depends on how severe your symptoms are, but you can improve the relationship between your pelvic floor and orgasms, reduce overflow incontinence (because bringing a spare pair of knickers around with you isn’t ideal!) and more. You can even practice Kegels during pregnancy to strengthen your pelvic floor as your bump grows.
How long do Kegels take to work?
Practicing pelvic floor therapy at home is a convenient and effective way of improving your pelvic health. But, it’s not a quick fix option. So, how long will it take to see results from kegels? The key is being consistent with your Kegel exercises — you should aim for three sets of five repetitions each day — and if you’re using our Elvie Trainer to improve your Kegel training routine, it’s best to use it three times a week minimum.
Natural home remedies to strengthen pelvic floor muscles
In addition to Kegel exercises, there are a number of other at-home remedies you can use to help combat pelvic floor dyssynergia. These include:
Yoga: By engaging the pelvic muscles as well as the abdominals, obliques and diaphragm, yoga is an effective way of increasing the strength of the pelvic floor muscles when introduced alongside Kegel exercises. Recommended yoga poses for those with pelvic floor disorders in child’s pose and ‘legs up the wall’.
Ab and core exercises: In addition to Kegels, you can engage the pelvic muscles through core exercises such as bridges, wall squats and jumping jacks. These are particularly effective if you’re looking for a slightly more challenging workout to do alongside other pelvic floor exercises.
Biofeedback: The technology that powers the Elvie Trainer, biofeedback is a technique which enhances pelvic floor workouts by recording information about muscle activity and then using this information to guide you on how to perform pelvic floor exercises more effectively.
Breathing exercises: You can help to increase pelvic floor strength and reduce pelvic pain by practicing breathing exercises. As you breathe in, try to relax the muscles completely, and then contract the muscles in an upward motion when you breathe out again.
Bladder training: Bladder control techniques involve trying to ‘train’ yourself to go to the bathroom at predetermined times — for example, once every 2 to 4 hours. This can help with pelvic muscle control and reduce urinary incontinence.
Depending on the severity of your pelvic floor dysfunction symptoms, you may also be recommended for pelvic floor physical therapy. A therapist will assess the muscles in your lower back, pelvis and pelvic floor, and then recommend a series of specific exercises to help improve strength and coordination.
Elvie Trainer to the rescue
With 1 in every 3 women experiencing pelvic floor problems during their lifetime, the award-winning Elvie Trainer is a fun yet highly-effective tool for building pelvic floor strength, helping you get to the core of any issues you might be facing.
Elvie Trainer uses something called biofeedback to measure your pelvic floor movements in real-time and lets you know when you’re not getting it quite right, enabling you to master your technique and get the most out of your Kegel workouts.
References
[1] I. Nygaard, M.D. Barber, K.L. Burgio, K. Kenton, S. Meikle, J. Schaffer, et al.
Prevalence of symptomatic pelvic floor disorders in US women JAMA, 300 (2008), pp. 1311-1316











 7 minute read
7 minute read